A team led by Prof. Tzu-Ming LIU in the University of Macau (UM) Faculty of Health Sciences (FHS), has made a breakthrough in the diagnosis of acute mesenteric ischemia (AMI). The study found riboflavin (vitamin B2) is a new diagnostic biomarker that correlates with the duration of intestinal ischemia and the degree of damage to the small intestine. The plasma fluorescence assay takes less than 2 minutes to perform, far less than the traditional biomarker assays which can take 2-4 hours., contributing to an efficient early screening. This technique is applicable to other severe diagnostic fields. The results have been published in the international journal Thrombosis Research.
AMI is a clinical syndrome of structural damage and dysfunction of the small intestine due to interruption of intestinal blood flow by embolism, thrombosis, or a low-flow state. Because its clinical symptoms are easily confused with other intestinal inflammatory diseases, delayed diagnosis leads to a 60-80% mortality rate. Clinical data demonstrate that failure in sensitively and accurately predicting the onset of AMI early can delay diagnosis and treatment, allowing the cytokine storm to expand and triggering systemic response syndrome and multi-organ failure. Late diagnosis is the most significant factor contributing to the high mortality rate associated with acute mesenteric ischemia. Therefore, providing early warning and accurate prediction of the AMI disease remains a critical scientific problem in critical care medicine for patients with acute abdominal pain. Doing so helps avoid increased mortality from delayed diagnosis and treatment.
Currently, the clinical diagnosis of AMI heavily relies on CT imaging. Although some markers, such as intestinal fatty acid binding protein, have been developed for sensitive detection, their quantification is still unreliable due to significant individual variations in baseline levels. CT imaging can only confirm the diagnosis of AMI in the late stage of the disease, resulting in consistently high mortality rates. To address this issue, the research team has proposed a fluorescence diagnosis method without reagents to reduce the time needed for early diagnosis and avoid delaying treatment and management.
The method involves exciting blood fluorescence at different wavelengths. The research shows that the intestine of AMI rats releases a significant amount of autofluorescent riboflavin into the bloodstream, which can evaluate disease development by monitoring the fluorescence intensity of riboflavin in plasma. The intensity of riboflavin fluorescence is proportional to the duration of ischemia, and the ratio of fluorescence intensity of two different fluorescent molecules (flavin/NADH) can reflect the onset of shock. The plasma fluorescence assay takes less than 2 minutes to perform, eliminating the need for additional reagents and providing a significant time advantage over traditional biomarker assays, which can take 2-4 hours. This method has made an important clinical implications for avoiding delayed diagnosis of acute mesenteric ischemia and reducing mortality.
Prof. Liu is the corresponding author of the study, PhD student Xueqin WU from UM is the first author, PhD student Lun-Zhang GUO and Yi-Hung LIU from Taiwan University are the co-first author. Others who have contributed to the study include former research assistant Yu-Cheng LIU of UM FHS, Prof. Hwan-Ching TAI from Xiamen University, Doctors Chao-Lun LAI, Yueh-Hsun CHUANG, Professors Tzung-Dau WANG, Pi-Tai CHOU and I-Rue LAI from Taiwan University. The project was supported by The Science and Technology Development Fund, Macao SAR (File No.: 122/2016/A3, 018/2017/A1, 0011/2019/AKP, 0120/2020/A3, 0026/2021/A), UM (File No.: MYRG2018-00070- FHS). The full version of the research article can be viewed at https://www.sciencedirect.com/science/article/pii/S0049384823000397?via%3Dihub.
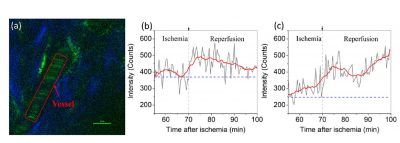
(a) In vivo two-photon image (λex = 920) mapped collagens (SHG, blue color) and yellow fluorescence (TPF, green color) in a rat’s ear. Scale bar: 10 μm. (b) and (c) are time-course flavin fluorescence intensities measured from the vessel area (red rectangle in (a)) of two rats. Blue dashed lines indicate the baseline intensities of each rat. The arrows indicate the starting time of reperfusion.
Tzu-Ming LIU(first row, middle), Xueqin WU (first row, 3rd from right )

